
It has been evident for decades that the fee-for-service (FFS) reimbursement model creates unsustainable financial incentives. The modern shift from a FFS contracting base to a fee-for-value one has been gaining momentum within the healthcare ecosystem, especially over the past five years.
Providers can no longer afford to maintain their FFS structure without engaging in some type of value component across all lines of business and this has never been more evident than in the most recent pandemic crisis of 2020. But what does the phrase “move to value” actually mean? And, what does it produce?
Instead of viewing it as a destination, the value journey is a continuously evolving improvement cycle along a spectrum of significant pillars of healthcare, including reimbursement models, driving appropriate utilization, improving outcomes, and patient satisfaction. The major milestones within this journey may include the following:
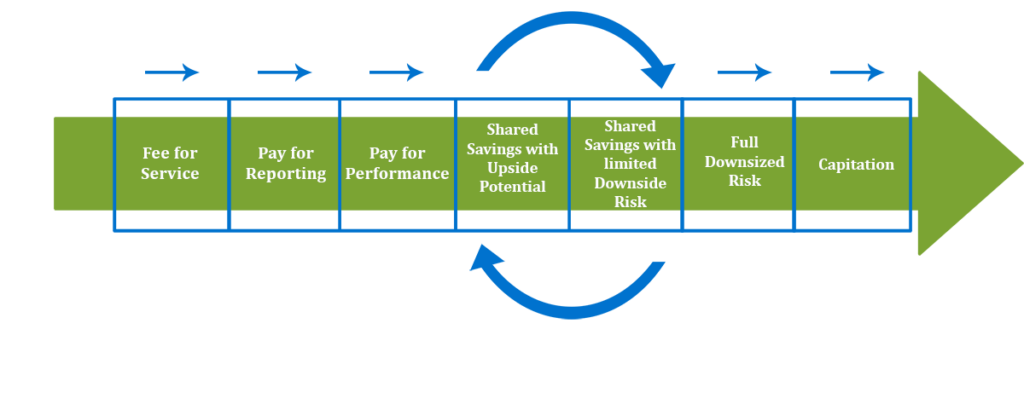
- Fee for Service: Reimburses providers for services rendered based on a set fee schedule. Attention is paid to the quantity of services provided, rather than necessary services.
- Pay for Reporting: Incentivizes providers to report quality information about the patient population, but does not require a certain threshold of quality measure performance.
- Pay for Performance: Incentivizes the provider to report quality information and establishes quality performance thresholds the provider must meet to unlock dollars. This structure does not take into account any type of cost management.
- Shared Savings with Upside Potential: Engages the provider to look at both the quality measure thresholds and total cost management of the patient population, typically through a Medical Loss Ratio or cost trend basis. The provider will share in a percentage in any savings generated for the patient population, but will not have to repay any attributed losses.
- Shared savings with Downside Risk: Allows the provider to share in an increased amount of the shared savings generated, but the provider will have to pay back a portion of any losses accrued.
- Full Downside Risk: The provider will retain 100% if any savings were generated, but would also have to repay 100% of the financial costs if medical expenses exceed the allotted amount to manage the population. These above models still operate on a Fee for Service foundation, but with an added layer of incentive to focus on quality and cost.
- Capitation: Combines value-based payment and fee for service by becoming one stream of revenue. In capitation, the provider receives a set amount of money on a recurring basis to take care of patients. Quality and cost of care still play a role.
Expanding and Innovating Payer Operations
The Centers for Medicare & Medicaid Services (CMS) and Health Plans have evolved within this value journey as well, whether it includes the development of new models, or investments in cost management techniques. Recently, CMS has unveiled its most aggressive traditional Medicare risk-sharing model called Direct Contracting , which allows new entities to take on full capitation for the Medicare beneficiaries they serve most.
“Health Plans continue to look for new investment options beyond financial reimbursement structures to affect the cost management space for their patients.“
Similarly, Health Plans continue to look for new investment options beyond financial reimbursement structures to affect the cost management space for their patients. Examples include social determinants of health platforms, post-acute care, chronic disease management, and palliative care.
Value Based Contracting Team Strategy
Innovation is happening all over the country. However, as “all healthcare is local,” an effective contracting team is well immersed in both the organization’s strategic goals and the operations team’s ability to closely monitorial the needs of the local market.
Contracting teams must first be aware of developments and innovations affecting the value based journey, both internally and externally, that are unique to each organization. Secondly, the contracting team must align the contracts with these strategic goals and the organization’s appetite for risk and current performance.
Internally, an organization must operate in close coordination with its operations team on the proposed contract or model requirements. The operations team best understands the organization’s ability to meet contract requirements from a day-to-day standpoint.
Value based contract support spans a broad discipline set ranging from assessing the technical and work flow specifics to support and capture discrete performance criteria, to determining appropriate risk levels for current and future years of participation. The contracting team must evaluate the financial investment needed for successful implementation (staff, technical needs, reserve establishment and/or stop loss), and the adaptability of the provider culture to engage in the value movement through education.
Once the contract is executed, the operations team can drive performance through its particular organizational structure and resources.
Externally, a contracting team needs to be involved in monitoring market development through as many avenues as possible. For example, the contracting team can stay abreast of developments by monitoring trade associations and professional organizations can provide insight into market developments, engaging with payer partners to understand developments beyond your immediate region, consulting with like-minded health systems to understand common or distinct challenges, and encouraging a culture of growth and advancement.
“Emphasize the organization’s need to focus on engagement and education about the value journey for all staff. This will promote early adoption, which is critical to success.”
Finally, emphasize the organization’s need to focus on engagement and education about the value journey for all staff. This will promote early adoption, which is critical to success. Provider and employee commitment levels must rise to meet the demand of continuous improvement. Start these conversations early and be intentional with the long-term strategy to move to value.
Aligning the company’s strategic vision with the value based model contract terms, and ensuring that the operations teams can execute those terms, will make for the surest footing as you begin the journey down the value-based path.
About the Authors

Bethany Palmer
Director of Network Management

Melissa Pollock, M.Div., CHC
Compliance and ACO Manager


