With North Carolina expanding Medicaid in late 2023, more low-income adults now have access to health coverage. But that access comes with new strings attached. North Carolina has moved forward with legislation to introduce work and community engagement requirements for certain NC Medicaid recipients, and federal rules set to take effect in 2027 will likely make such requirements mandatory.
Healthcare workers and managed Medicaid teams will play a key role in explaining these changes, both to providers and directly to patients. What follows is a clear, straightforward guide to help you prepare.
The Basics: What’s Changing
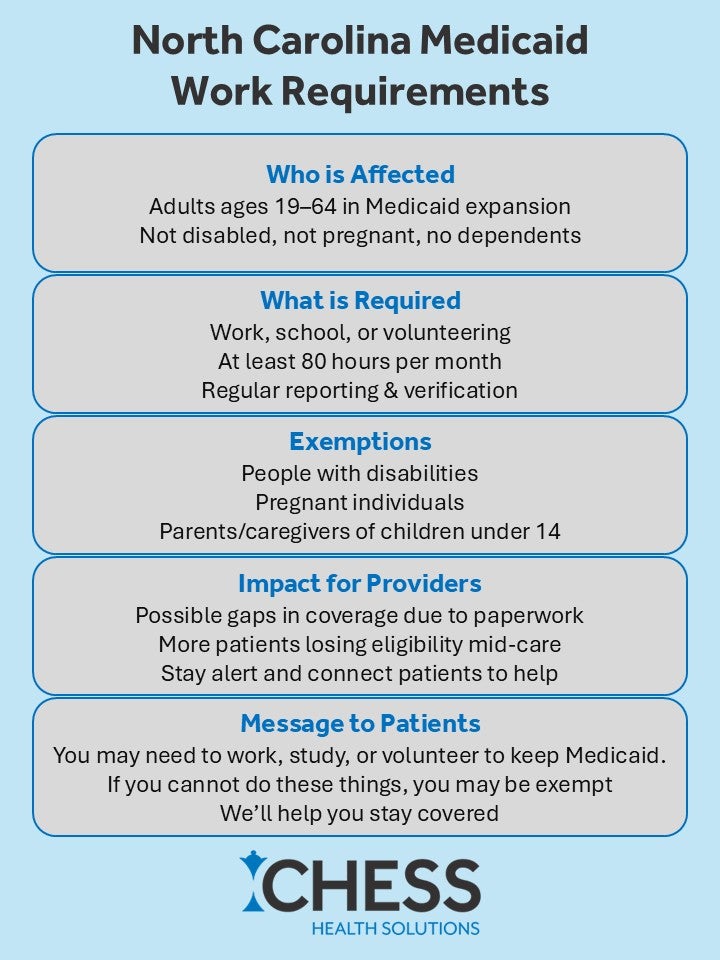
Work requirements will likely apply to adults in the expansion population: those aged 19 to 64 who are not disabled and do not have dependent children. These individuals will be required to participate in work, education, job training, or volunteering for at least 80 hours per month. They will also need to regularly report and verify their activities to maintain coverage.
Some patients will be exempt, including those who are pregnant, have disabilities, or care for young children. But for everyone else, failing to meet the requirement, or the inability to prove they’ve met it, could mean losing Medicaid coverage.
These requirements are not in effect yet, but the groundwork is being laid, and the federal timeline points to January 2027 as a likely rollout date.
Talking to Providers: Focus on Care Disruption
Providers don’t need every detail, but they do need to understand how these requirements could affect their patients and workflows.
Start by explaining that coverage interruptions are likely. Many patients will lose coverage not because they fail to work, but because they don’t understand the rules or miss a paperwork deadline. That can lead to gaps in care, missed appointments, or delays in getting medications approved.
Encourage providers to be proactive. They should check Medicaid status at every visit, stay alert to changes in insurance coverage, and refer patients to Medicaid navigators or care coordinators when questions arise. Also, let them know that administrative burdens may increase as more patients need documentation, letters, or support to prove their eligibility.
A short, clear explanation might go like this:
“Some of your Medicaid patients may soon need to show they’re working or in school to keep their coverage. This could cause disruptions if patients lose eligibility mid-treatment. Let us know if you have patients at risk; we can help them stay covered.”
Talking to Patients: Keep It Simple, Supportive, and Clear
The conversation with patients should be even more direct, with an emphasis on support and reassurance.
Don’t lead with legal language or complex rules. Focus on what the patient needs to know and do. For example:
“In the next year or two, some NC Medicaid patients will need to work, go to school, or volunteer a few hours a week to keep their insurance. If that includes you, we’ll help you stay on track.”
Make it clear they won’t have to navigate this alone. If they cannot work because of health issues or family responsibilities, they may be exempt. The most important thing is that they communicate with NC Medicaid, provide the right paperwork, and ask for help if they’re confused.
Use patient navigators, social workers, or Medicaid enrollment specialists whenever possible to help guide patients through these conversations. Confusion and fear will be common, especially among those already struggling to meet basic needs. The message should be calm, practical, and empathetic.
What to Do Now
Even before the rules are official, there is value in preparing. Start identifying who on your panel might be affected, especially single adults without children. Train your front-desk and call center staff to recognize Medicaid red flags and refer patients to internal resources. Stay current on state guidance as it evolves.
The shift toward work requirements represents more than a policy change—it’s a new layer of complexity in delivering care. Your role is to keep coverage intact, care consistent, and communication clear.
If we do this right, patients won’t just stay insured; they’ll stay healthy.