
Imagine this scenario: today you saw one of your established patients, who is usually in a pleasant and talkative mood, but something was different. At first, they were quiet, only answering questions with a yes or no response and seemed to be avoiding any direct eye contact. They appeared tired and looked like they had lost weight. How do you determine HCC coding?
Once you started asking questions about their appearance, the patient starting crying and revealed that since the last visit 6 months ago, their spouse of 30 years was diagnosed with lung cancer and bone metastasis and was given a life expectancy of 3 months.
Diagnosis specificity goes beyond reimbursement. In this case, supporting documentation and the further specified diagnosis lets everyone else know the patient’s acuity.
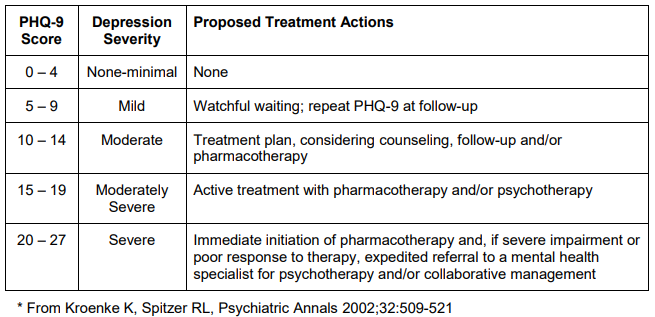
You review the PHQ-9 questionnaire and see a score of 25. In your note, you document the patient’s symptoms along with a diagnosis of depression; make a referral for follow up care; start the patient on an antidepressant to help with the symptoms; and schedule a follow up visit in 3 weeks to assess the effectiveness of the medication.
It looks like you covered all your bases, but before you close out that chart, pause for a minute and consider the following questions:
Did you know “Depression” codes to Depression, Unspecified and does not reflect the severity or episode of the disorder?
- Does your diagnosis accurately reflect the acuity or severity of depression for the patient?
- Does the diagnosis reflect the resources a care coordination team may utilize to make sure the patient receives the appropriate follow up care or interventions?
- Does the diagnosis support the need for a referral or the medication you prescribed?
- Does the diagnosis of “depression” support the E/M level of service?
- Is a treatment plan, pharmacotherapy, and/or psychotherapy recommended on the PHQ-9 for a diagnosis of “depression”?
Diagnosis specificity goes beyond reimbursement. In this case, your supporting documentation and the further specified diagnosis of “Major depressive disorder, single episode, moderate or severe without psychotic features” lets everyone else know the acuity of the patient’s depression. It also provides the medical necessity for additional resources, medications, referrals, and follow-ups. It also justifies the additional costs of caring for this patient versus someone feeling “blue” or with mild depression.
Depressive Disorder
HCC Coding: Major Depressive Disorder
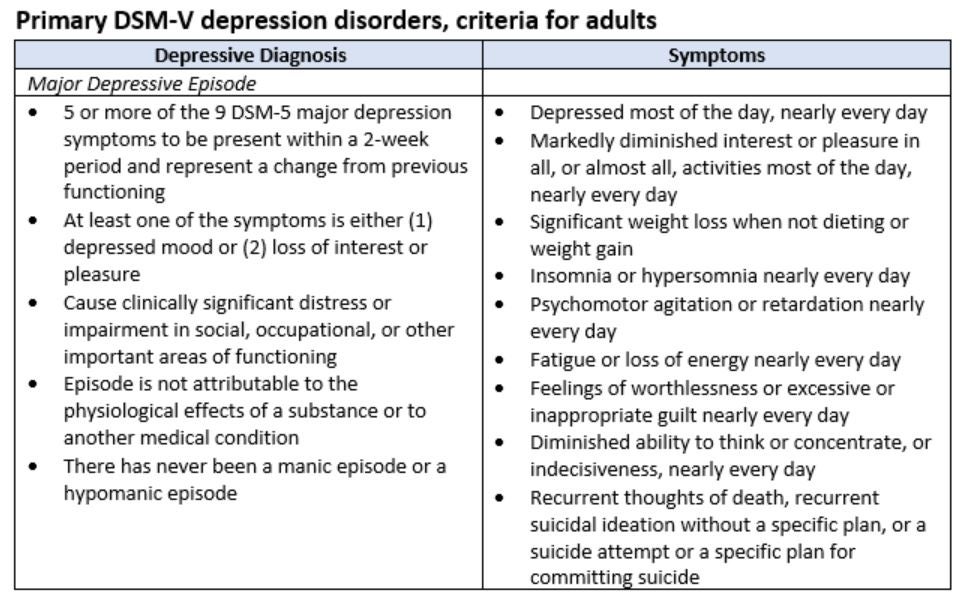
Three things need to be documented to appropriately capture the severity of illness of your patients who suffer from depression:
- Episode
- Single
- Recurrent
- Activity
- Not in remission
- Partial remission
- Full remission
- If not in remission, please document the severity
- Mild
- Moderate
- Severe
- If severe, please document any complications
- With psychotic features
- Without psychotic features
- If severe, please document any complications
Good diagnosis documentation examples:
- “Major depression, recurrent, in remission”
- “Moderate recurrent major depression”
- “Major depression, single severe episode with psychotic features”
*Note: Assumed not to be in remission if severity of episode graded
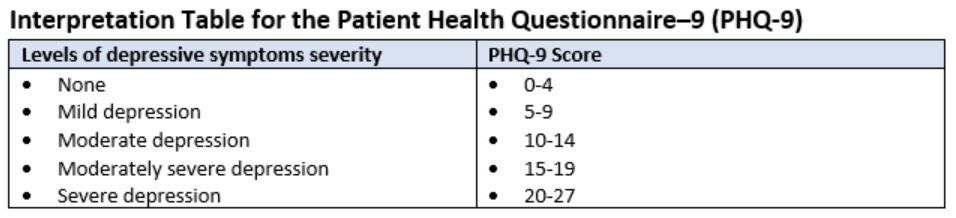
Interpretation Table for the Patient Health Questionnaire–9 (PHQ-9)
Table 4. PHQ-9 Scores and Proposed Treatment Actions *
The full PHQ, Brief PHQ, and PHQ for Adolescents (PHQ-A) can be used to establish provisional diagnoses for selected DSM-IV disorders. The diagnostic algorithm for the PHQ modules are included in footers at the bottom of each page of the PHQ, and also reiterated in Table 2, page 4. The other measures are principally used to derive severity scores (PHQ-9 and PHQ-8 for depressive symptom severity; GAD-7 for anxiety symptom severity; PHQ-15 for somatic symptom severity) or as ultra-brief screeners (PHQ-2, GAD-2, PHQ-4).

