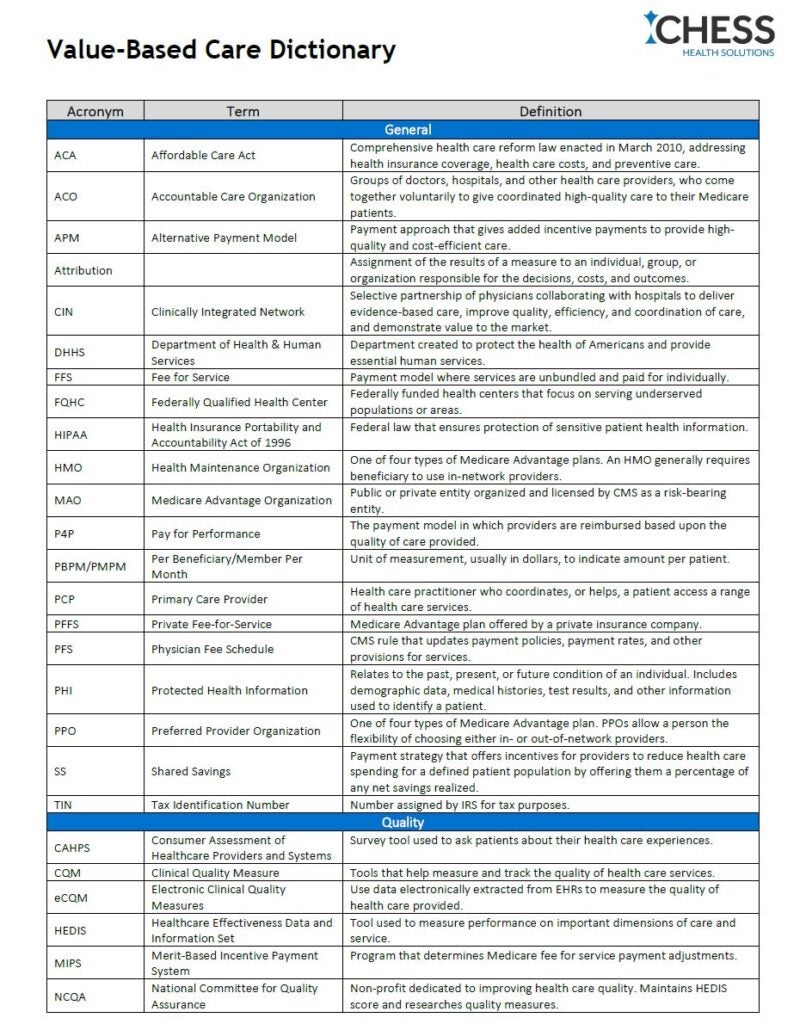
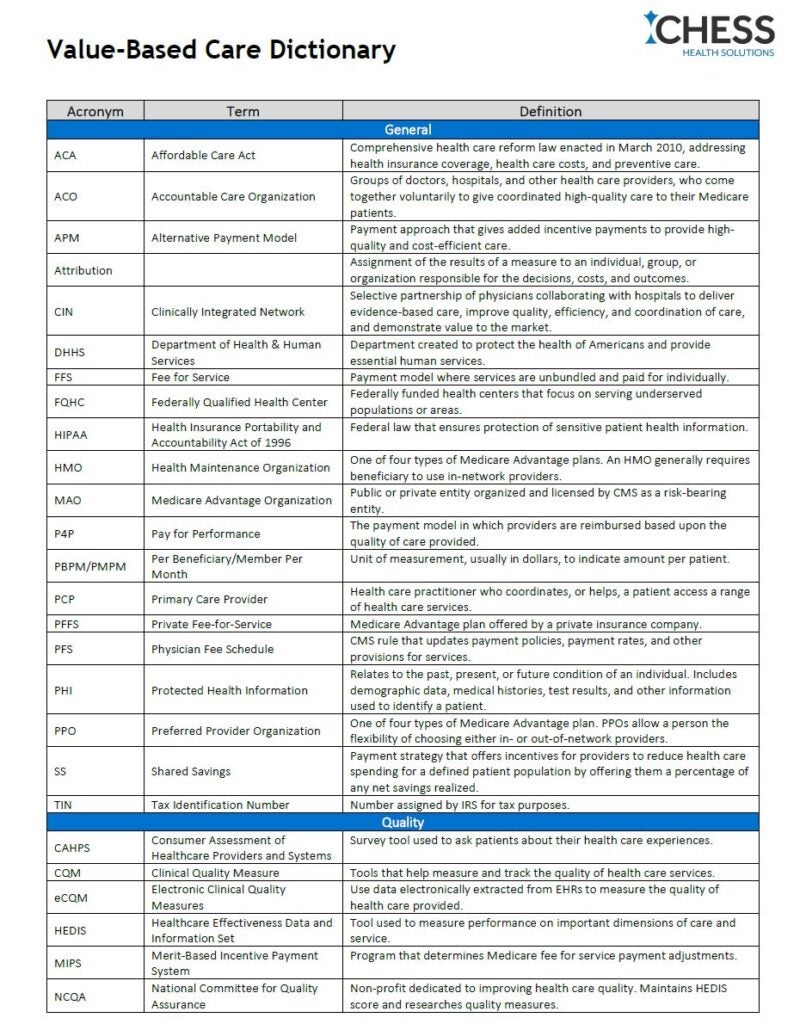
Download Value-Based Care Dictionary pdf here
General
| ACA | Affordable Care Act | Comprehensive health care reform law enacted in March 2010, addressing health insurance coverage, health care costs, and preventive care. |
| ACO | Accountable Care Organization | Groups of doctors, hospitals, and other health care providers, who come together voluntarily to give coordinated high-quality care to their Medicare patients. |
| APM | Alternative Payment Model | Payment approach that gives added incentive payments to provide high-quality and cost-efficient care. |
| Attribution | Assignment of the results of a measure to an individual, group, or organization responsible for the decisions, costs, and outcomes. | |
| CIN | Clinically Integrated Network | Selective partnership of physicians collaborating with hospitals to deliver evidence-based care, improve quality, efficiency, and coordination of care, and demonstrate value to the market. |
| DHHS | Department of Health & Human Services | Department created to protect the health of Americans and provide essential human services. |
| FFS | Fee for Service | Payment model where services are unbundled and paid for individually. |
| FQHC | Federally Qualified Health Center | Federally funded health centers that focus on serving underserved populations or areas. |
| HIPAA | Health Insurance Portability and Accountability Act of 1996 | Federal law that ensures protection of sensitive patient health information. |
| HMO | Health Maintenance Organization | One of four types of Medicare Advantage plans. An HMO generally requires beneficiary to use in-network providers. |
| MAO | Medicare Advantage Organization | Public or private entity organized and licensed by CMS as a risk-bearing entity. |
| P4P | Pay for Performance | The payment model in which providers are reimbursed based upon the quality of care provided. |
| PBPM/PMPM | Per Beneficiary/Member Per Month | Unit of measurement, usually in dollars, to indicate amount per patient. |
| PCP | Primary Care Provider | Health care practitioner who coordinates, or helps, a patient access a range of health care services. |
| PFFS | Private Fee-for-Service | Medicare Advantage plan offered by a private insurance company. |
| PFS | Physician Fee Schedule | CMS rule that updates payment policies, payment rates, and other provisions for services. |
| PHI | Protected Health Information | Relates to the past, present, or future condition of an individual. Includes demographic data, medical histories, test results, and other information used to identify a patient. |
| PPO | Preferred Provider Organization | One of four types of Medicare Advantage plan. PPOs allow a person the flexibility of choosing either in- or out-of-network providers. |
| SS | Shared Savings | Payment strategy that offers incentives for providers to reduce health care spending for a defined patient population by offering them a percentage of any net savings realized. |
| TIN | Tax Identification Number | Number assigned by IRS for tax purposes. |
Quality
| CAHPS | Consumer Assessment of Healthcare Providers and Systems | Survey tool used to ask patients about their health care experiences. |
| CQM | Clinical Quality Measure | Tools that help measure and track the quality of health care services. |
| eCQM | Electronic Clinical Quality Measures | Use data electronically extracted from EHRs to measure the quality of health care provided. |
| HEDIS | Healthcare Effectiveness Data and Information Set | Tool used to measure performance on important dimensions of care and service. |
| MIPS | Merit-Based Incentive Payment System | Program that determines Medicare fee for service payment adjustments. |
| NCQA | National Committee for Quality Assurance | Non-profit dedicated to improving health care quality. Maintains HEDIS score and researches quality measures. |
| PMPM/PMPY | Per Member Per Month/Year | Refers to the dollar amount paid each month for each individual enrolled in a managed care plan, often referred to as capitation. |
| PY | Performance Year | 12-month period beginning during the agreement period, unless otherwise specified or noted in the contract. |
| RAR | Readmission Rate | Percentage of admitted patients who return to the hospital within 7 days of discharge. |
| WIQM | Web Interface Quality Measure | Clinical quality measures reported by an ACO to Medicare based on the patient population. |
Clinical
| ASC | Ambulatory Surgical Center | Health care facility providing same-day surgical care. |
| ACSC | Ambulatory Care Sensitive Conditions | Conditions for which hospital admission could be prevented by timely and effective outpatient care. |
| APC | Advanced Practice Clinician | Includes advanced practice registered nurses and physician assistants. |
| APP | Advanced Practice Provider | Provider who is not a physician but performs medical activities typically performed by a physician. Most commonly a nurse practitioner or physician assistant. |
| AWV | Annual Wellness Visit | Medicare covers the AWV, a preventive wellness visit. |
| CCM | Chronic Care Management | Non-face-to-face services provided to Medicare beneficiaries who have multiple (two or more) significant chronic conditions. |
| DTP | Drug Therapy Problems | Clinical problems related to the use of medications. |
| EHR | Electronic Health Record | Electronic database that stores confidential patient information. |
| EMR | Electronic Medical Record | Digital version of a patient’s chart. |
| SNF | Skilled Nursing Facility | In-patient rehabilitation and medical treatment center staffed with trained medical professions. |
| TCM | Transitional Care Management | Services that address the hand-off period between inpatient and community settings. |
| TOC | Transitions of Care | Process of transferring a patient’s care from one setting or level of care to another. |
| SDOH | Social Determinants of Health | Conditions in the places where people are born, live, learn, and work that affect a wide range of health, functioning, and quality-of-life outcomes and risks. |
| HPI | History of Present Illness | Description of development of patient’s present illness. |
| LTC | Long Term Care | Services to meet needs of people with chronic illness or disability who cannot care for themselves for long periods. |
Coding
| CDI | Clinical Documentation Improvement | Process of improving health care records to ensure improved patient outcomes, data quality, and accurate reimbursement. |
| HCC | Hierarchical Condition Category | Medical codes linked to specific clinical diagnoses. |
| ICD-11 | International Classification of Diseases | Medical classification list by the World Health Organization. |
| RADV Audits | Risk Adjustment Data Validation Audits | Process of verifying diagnosis codes submitted for payment with the support of medical record documentation. |
| RAF | Risk Adjustment Factor | Medical risk adjustment model used by CMS to represent a patient’s health status. |
CMS
| CMS | Centers for Medicare and Medicaid Services | Federal agency responsible for administering Medicare and overseeing state administration of Medicaid. |
| CMMI | Center for Medicare & Medicaid Innovation | The innovation center was created for the purpose of testing “innovative payment and service delivery models to reduce program expenditures…while preserving or enhancing the quality of care.” |
| GPDC | Global and Professional Direct Contracting Model | Set of two voluntary risk-sharing options aimed at reducing expenditures and preserving quality of care for beneficiaries in Medicare FFS. |
| MA | Medicare Advantage | Type of Medicare health plan offered by a private company that contracts with Medicare to provide Part A and B benefits. |
| MACRA | Medicare Access and CHIP Reauthorization Act of 2015 | Changed how Medicare pays physicians who provide care to Medicare beneficiaries. |
| MBI | Medicare Beneficiary Identifier | Every person with traditional Medicare is assigned an MBI. |
| MBR/MLR/MER | Medical Benefit Ratio Medical Loss Ratio Medical Expense Ratio | Amount of premium revenue spent on medical care and services. |
| MIPPA | Medicare Improvements for Patients and Providers Act of 2008 | Supports states through grants to provide outreach and assistance to eligible Medicare beneficiaries to apply for benefits programs that help lower cost of their premiums and deductibles. |
| MIPS | Merit-Based Incentive Payment System | One option of the MACRA Quality Payment Program. Comprised of quality, cost, improvement activities, and advanced care information. |
| MSPB | Medicare Spending per Beneficiary | Assesses Medicare Part A and Part B payments for services provided to a Medicare beneficiary during a spending-per-beneficiary episode. Evaluates hospitals’ efficiency relative to the efficiency of the median hospital. |
| MSSP | Medicare Shared Savings Program | Voluntary program that encourages doctors, hospitals, and other health care providers to come together as an ACO to give coordinated, high quality care to their Medicare beneficiaries. |
| NGACO | NextGen or Next Generation | Initiative for ACOs that were experienced in coordinating care for Medicare populations. It allowed these provider groups to assume higher levels of financial risk and reward. |
Data + Tech
| CDS | Clinical Decision Support | A health IT system that is designed to provide physicians with clinical decision-making tasks. |
| CEHRT | Certified Electronic Health Record Technology | EHR that’s demonstrated the tech capability, functionality, and security requirements required by DHHS. |
| HIE | Health Information Exchange | Use of technology to manage current and historical information related to a person’s care. |
| HIT | Health Information Technology | The exchange of health information electronically, with the goal of improving quality of care by reducing costs, errors, and inefficiency. |