
Engaged patients lead to significant benefits. Patient engagement decreases utilization, improves outcomes, and increases patient satisfaction, all while lowering healthcare costs. Healthcare professionals can use motivational interviewing (MI) to engage and empower patients in their healthcare journey, reducing risky behaviors and promoting healthy behaviors.
MI puts behavior change in the hands of the patient. It is a collaborative, goal-oriented style of communication that emphasizes partnership and compassion. At the heart of MI is the ability to empathize with patients rather than being directive. By eliciting the patient to use their own motivation to change, a healthcare professional guides the patient towards change, rather than directing them to change. Research has shown that a patient’s personal motivation for change is far more influential than a lecture from a clinician.
Guiding principles of MI include:
- Resist the “righting reflex” or the urge to correct
- Use active listening to engage with the patient
- Understand the patient’s motivations for change
- Ask powerful open-ended questions
- Honor the patient’s values
- Respect patient’s freedom to choose
- Partnership-like collaboration
- Clinician should not assume the role of the expert
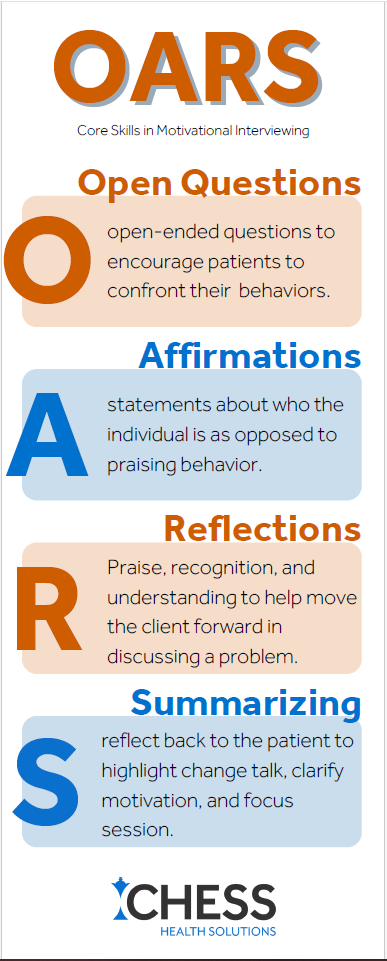
Structuring conversations using OARS will put behavior change goals in the hands of the patient, leading to successful MI.
O – open ended questions
These questions cannot be answered with a simple “yes” or “no.” Rather than asking “do you see a connection between your smoking and recent high blood pressure,” try asking “what is your understanding of the relationship between smoking and high blood pressure.” Starting questions with what, how well, tell me more about, etc. will uncover key information without asking a patient to justify a decision or behavior.
A – affirmations
Affirmations build rapport, demonstrate empathy, and build a patient’s self-efficacy. Affirmations require listening to what a patient is saying and finding opportunities to acknowledge past decisions, abilities, and healthy behaviors. These statements are more about the individual as opposed to praising behavior. For example, “I really appreciate that you are willing to come into the clinic this morning,” or “you handled yourself very well in that situation.”
R – reflections
Reflections help move the client forward in discussing a problem. Reflections let the patient hear their behaviors, words, and feelings mirrored back, boosting awareness. Clinicians can repeat the patient’s words, reflect what the patient is feeling, state an observation, or reframe.
S – summarizing
Summarizing, which includes paraphrasing, is a way to transition and close conversations. At the end of a session, it will help to review the patient’s action plan.
By identifying obstacles, solutions, and a clear plan, healthcare providers can help patients tap into their own motivation to change. When the motivation for change comes from the patient, a successful transformation is more likely to occur.
Download a PDF Overview of the OARS Method Here
RESOURCES: AAFP, AHRQ, https://www.oregon.gov/oha/ph/HealthyPeopleFamilies/ReproductiveSexualHealth/Documents/edmat/OARSEssentialCommunicationTechniques.pdf

