
In documents published on the CMS website, dated March 17, additional Telehealth services have been authorized expanded coverage for Telemedicine services as part of the Coronavirus Preparedness and Response Supplemental Appropriations Act. Listed below are the key takeaways. The link for the Provider Fact Sheet is: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
Expansion of Telehealth with 1135 Waiver
Under this waiver, Medicare can pay for office, hospital and other visits furnished via telehealth, including patients’ places of residence. The HHS Office of Inspector General is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs.
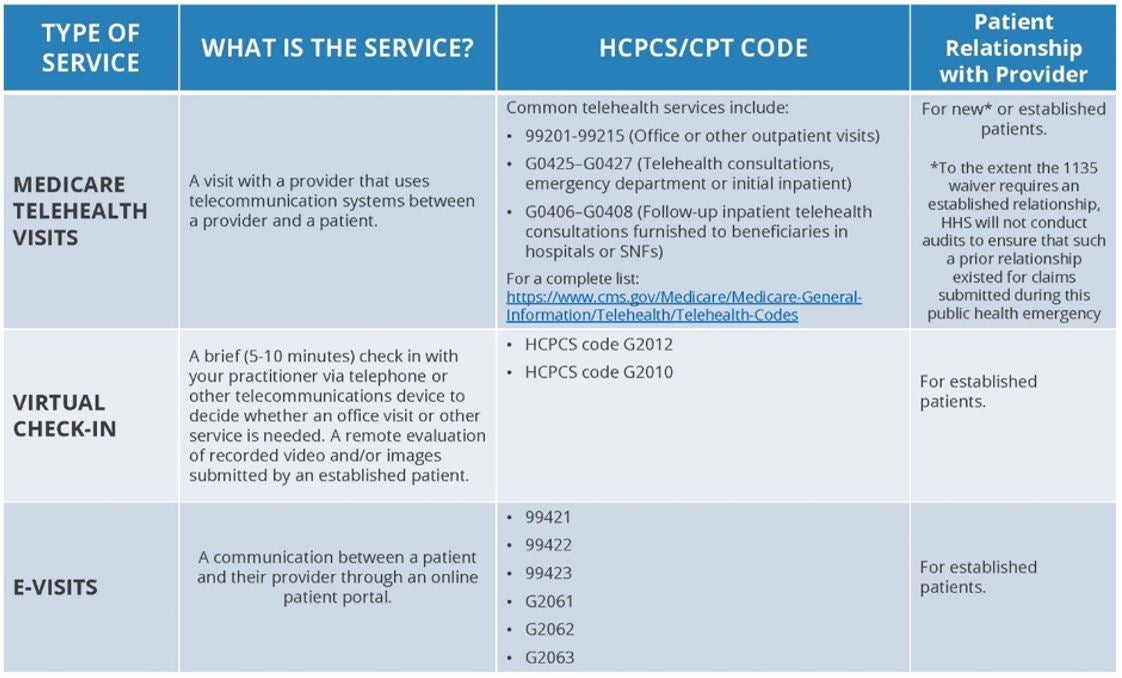
Medicare Telehealth Visits
- The provider must use an interactive audio and video telecommunications system that permits real-time communication between the distant site (where the provider is located) and the patient at home. Distant site providers who can furnish and receive payment for covered telehealth services (subject to state law) include physicians, nurse practitioners, physician assistants, nurse midwives, certified nurse anesthetists, clinical psychologists, clinical social workers, registered dietitians, and nutrition professionals.
- These visits are considered the same as in-person visits and are paid at the same rate as regular in-person visits. For the duration of the COVID-19 Public Health Emergency, Medicare will make payment for professional services furnished to beneficiaries in all areas of the country in all settings.
- The goal of this waiver is to avoid travel, when possible, to offices, clinics, hospitals or other healthcare facilities. While the waiver requires that the patient have a prior relationship with a specific provider for telehealth services, HHS will NOT conduct audits to ensure that such a prior relationship existed for claims submitted during this public health emergency.
Virtual Check-In Visits
- Established Medicare patients in their home may have a brief communication service with providers via a variety of communication technology modalities, including synchronous discussion over a telephone or exchange of information through video or image. CMS expects these virtual services will be patient-initiated, but providers may need to educate beneficiaries on availability of the service prior to patient initiation.
- The communication may not be related to a medical visit within the previous seven (7) days and does not lead to an in-person visit within the following 24 hours/first available appointment of the check-in visit. If either of those situations occur, you may not bill the virtual “check-in” visit. For our Palmetto MAC, the 2020 fee schedule pays HCPCS G2012, telephonic check-in, $14.27; and HCPCS G2010, captured video check-in, $11.80 (facility fees not included). The beneficiary may be located in his/her home for these visits. These are for established patients with a provider/practice. Deductibles and co-insurance fees apply.
E-Visits
In all types of locations, including the patient’s home, and all areas, established Medicare patients may have non-face-to-face patient-initiated communications with their providers without traveling to the office by using on-line patient portals. These services may only be reported when the billing practice has an established relationship with the patient. For these E-Visits, the patient must initiate the inquiry and communications can occur over a 7-day period. The services are billed using CPT codes 99421-99423 and HCPCS Codes G2061-G2063. Medicare co-insurance and deductibles apply to these services.
Practitioners who may independently bill Medicare for E/M visits (i.e., physicians and nurse practitioners) can bill the following codes:
- 99421 – Online, digital E/M service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5-10 minutes.
- 99422 – Online, digital E/M service, for an established patient, for up to 7 days cumulative time during the 7 days; 11-20 minutes.
- 99423 – Online digital E/M service, for an established patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes.
Clinicians who may not independently bill for E/M visits (e.g, physical therapists, occupational therapists, speck language pathologists, clinical psychologists) can also provide these E-visits and bill the following codes:
- G2061 – Qualified non-physician healthcare professional online assessment and management for an established patient, for up to 7 days, cumulative time during the 7 days; 5-10 minutes.
- G2062 – – Qualified non-physician healthcare professional online assessment and management for an established patient, for up to 7 days, cumulative time during the 7 days; 11-20 minutes.
- G2063 – – Qualified non-physician healthcare professional online assessment and management for an established patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes.
About the Author


